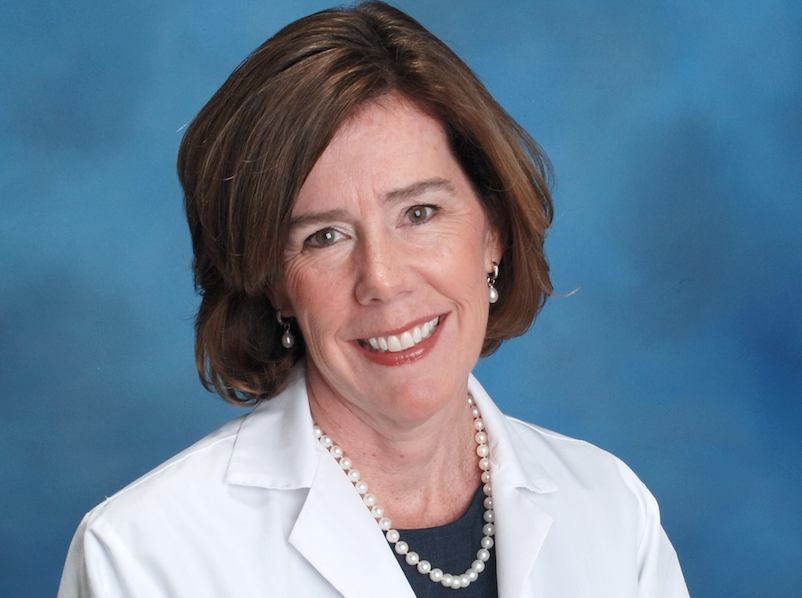
How did you choose your infectious disease specialty when you entered the medical field?
I loved all of medicine so it was not an easy decision. It turned out that the doctors who taught me and made the biggest impression during my residency were infectious diseases docs. Because I wanted to be like them, I think I gravitated to infectious diseases. Certainly I was very lucky and am so grateful to them for their mentorship and support. Infectious diseases docs care for a huge variety of patients, including those with skin infection, flu, pneumonia, and those with very unusual and life-threatening infections like malaria, TB, HIV and now COVID-19. We also have the opportunity to help cure people which is very gratifying.
How has the work you have been doing changed from before the covid-19 pandemic outbreak, to now?
My job has changed in a huge way. My team and I are all working 24×7 to care for COVID patients and help keep all our colleagues safe. Our job includes diagnosing, treating and preventing COVID infections. We work with colleagues all across the medical center to help them care for COVID patients safely. A big part of this is educating colleagues about infection prevention and how to use personal protective equipment, or PPE. This includes masks, eye protection and gloves that are very important to keep us all safe. As Chief of our Infectious Diseases Division, I attend numerous meetings with leaders to provide updates, help solve problems and provide education.
Could you describe an example of a day in life for you at work during this time?
My day begins at 7AM with a meeting in the Emergency Department to discuss new patients and plans for the day. At 7:30 I meet with the Infectious Diseases team to review the patients who came in overnight and plan for our 5 teams for the day. At 8AM we have the incident command center team meeting where leaders from across the hospital discuss everything from how many COVID patients we have to how our supplies are doing, to how we’ll set up new intensive care units to care for the incoming patients who need us. After that I work to prepare my daily report on the epidemic that is presented to a variety of groups. Sometimes I have another meeting with our infection prevention team at 8:30 or 9 to address a problem or need for the day. At 10AM we have a meeting for leaders across our healthcare system called Wellforce. Here we discuss the status of the epidemic across our hospitals and home health agency (this includes hospice patients). After that I have a meeting in the microbiology lab where we review the new results and discuss cases that need our input. Then I attend several more meetings where that report on the status of the epidemic is presented. I also may see a patient or a few patients who have urgent problems either via telehealth or in person. I then round on the floors in the hospital to see how the teams are doing and help as needed. Later in the afternoon, I have other meetings with my team to assess progress during the day and plan for the next day. Most days I also speak with the press, either for radio or TV, to help educate the public about the epidemic. In the evening, there are yet more meetings focused on things including how we plan to expand testing and to care for patients who need us going forward. I also often meet with one or more of my 30 faculty members to discuss their research or other needs. We’ve also begun planning for “re-opening” the medical center. This involves thinking about how we’ll treat COVID-infected and non-COVID patients safely and how we’ll keep our community safe (precautions including PPE, etc.).
What do you expect will be the long-lasting effects of this pandemic after it is over?
I think and very much hope we’ll be better at staying prepared for the next pandemic. This means attending to things like developing tests and treatments for diseases we know are coming and even those we don’t yet know about. I also think we’ll come out of this slowly and in steps. It is possible that things like telehealth may stay with us and that may be a good thing.
How are you personally protecting yourself and your family from the virus?
Great question! The best protection is to wash your hands frequently, avoid touching your face, wipe down frequently touched surfaces (door knobs, handles, counters, etc.), stay home, especially when you’re sick, keep physical distance (at least 6 feet), and avoid large crowds. We are also wearing face covering in public to avoid passing along our germs (masks contain our cough so we won’t infect another person). As hard as this physical distancing is, we know that it works and it IS working! Lives have been saved by the hard work you are doing so keep it up!
Do you have any predictions about life in the future and when people will no longer need to distance themselves?
As I noted above, I think we will slowly come out of this with some type of graded relaxing of the physical distancing. I’ve heard ideas like breaking the school into groups who attend for part of the day to limit the number of people in the building at once. It is also likely that we’ll want to keep up some physical distancing for a while. For instance, it may be recommended that we not visit grandparents and other vulnerable people after returning to work/school to protect them.